Four Principles of Pain #
Minimum viable knowledge for working with pain.
I. Pain is not a measure of damage #
Most of us naively equate pain with tissue damage. The most common view is that pain is the body’s perception of damage. \[ \text{Tissue damage} \rightarrow \text{Pain receptors fire} \rightarrow \text{Experience of pain} \] \[ \text{or} \] \[ \text{Tissue damage} \implies \text{Pain} \]
This is why if you go into a doctor’s office reporting back pain, they will often image your spine for abnormalities (e.g. herniated disk or spinal stenosis)1. They can then attempt try to fix these abnormalities via surgery or, failing that, give you painkillers to manage the pain.
Unfortunately, this model is too simple. Pain does not strictly imply damage:
Many people have damage without pain.
Most pain-free people have some degree of spinal, hip, shoulder, and knee ‘abnormalities’.
In a famous 1994 study, MC Jensen et al. examined the MRI images of the backs of 98 pain-free people. Of the participants, aged twenty and older, over half had an abnormality (“damage”) in at least one disk2. Herniation or disk bulges were strikingly common in patients who were pain free.
Many follow up studies have replicated this. It is very common for pain-free people have structural damage in their hips, shoulders, and knees. For instance:
- Rajaswaran et al (2014) found spinal abnormalities (synovial cysts, disc degeneration and arthropathy) in 96% of pain free young athletes.
- Tresch et al (2016) found defects in the hip cartilage of 57% of pain-free 20-50 year olds.
- Templehof et al (1999) saw full rotator cuff tears in 23% of people reporting no pain.
Many people have pain without damage.
If you have a limb amputated, there’s about a 80% chance that you begin to feel major pain at the periphery of the amputed limb, years after the tissue around the limb has fully healed 3. People who experience this describe with incredible specificity the burning or shooting pains in their missing hands and feet. Although their tissue is not damaged, the pain is certainly real — the firsthand accounts are particularly convincing3.
Many forms of chronic pain are also associated with no tissue damage. The World Health Organization estimates that over 550 million people are affected by lower-back pain that can’t be explained by a disease or structural abnormality 4. Other examples of chronic pain with no associated damage include fibromyalgia 5, Irritable Bowel Syndrome, and many others.
There is more to pain than physical damage.
II. Pain is a generated signal for protective action #
If it’s not just a measure of physical damage, then what is pain?
\[ \text{Pain is a generated signal for protective action} \]How did pain evolve?
The neural circuitry for responding to harm evolved around 600 million years ago, in our great ancestor — the bilateral worm. It was a protective instinct responding to external stimuli; If poked, the worm would retreat6.
Initially, it was all instinct. Pain wasn’t ‘unpleasant’ because worms didn’t have the neural tissue for feelings. It was only much later, with the development of structures like the limbic system, that our ancestors began to have the unpleasant feelings that we would recognize as pain.
The purpose of pain is to get you to act.
Say you’re cooking later today and accidentally touch a burning stove. What do you do? You whip your hand away from the stove. You might cool it down under running water, and then you’ll keep it close to your body.
The pain hurts so that you move to safety. So you protect your hand from further damage. If the pain is bad enough, you’ll also learn to be more careful around stoves, and you might even be afraid of frying things.
Pain is a learning signal your nervous system generates for protective action. With it, you protect your hand, and avoid future situations where your hand is at risk.
Pain is generated from past experience
As with all signals that our body generates, it is heavily informed by past experience.
You can naively think about our experience as an integration of sensory stimuli and our expectations.
Three Views on Pain #
In more detail, here are three ways of understanding pain
Evolutionary Biology #
Pain as a learning signal for protective action.
Pain, from an evolutionary standpoint, represents a highly conserved biological mechanism that has undergone significant refinement over millions of years. Its origins can be traced back to primitive nociceptive reflexes in early bilateral organisms, evolving into the sophisticated, multi-layered experience observed in humans. This phylogenetic progression reflects the adaptive value of pain in promoting survival behaviors and reproductive fitness. The modern human pain experience, with its complex sensory, emotional, and cognitive components, is the result of successive evolutionary adaptations, each building upon earlier protective mechanisms to create a nuanced system for threat detection and response.
Computational Neuroscience #
Pain as a bodily inference that integrates prior experience, present sensory data, and the current context.
“In individuals with chronic pain harmless bodily sensations can elicit anticipatory fear of pain resulting in maladaptive responses such as taking pain medication. Here, we aim to broaden the perspective taking into account recent evidence that suggests that interoceptive perception is largely a construction of beliefs, which are based on past experience and that are kept in check by the actual state of the body. Taking a Bayesian perspective, we propose that individuals with chronic pain display a heightened prediction of pain [prior probability p(pain)], which results in heightened pain perception [posterior probability p(pain|sensation)] due to an assumed link between pain and a harmless bodily sensation [p(sensation|pain)]. This pain perception emerges because their mind infers pain as the most likely cause for the sensation. When confronted with a mismatch between predicted pain and a (harmless bodily) sensation, individuals with chronic pain try to minimize the mismatch most likely by active inference of pain or alternatively by an attentional shift away from the sensation.”
Hechler, Tanja, Dominik Endres, and Anna Thorwart. “Why harmless sensations might hurt in individuals with chronic pain: about heightened prediction and perception of pain in the mind.” Frontiers in psychology 7 (2016): 1638.
Complexity theory (and enactivism) #
Pain as an experience that arises at the intersection of environmental, social, biological, and psychological factors.
Complexity theory offers a paradigm for understanding pain as an emergent phenomenon arising from the nonlinear interactions within a complex adaptive system. This approach acknowledges the multifaceted nature of pain, incorporating biological, psychological, and social dimensions. Pain is viewed not as a simple input-output process, but as a dynamic state emerging from the intricate interplay of multiple factors across various scales of organization. This perspective emphasizes the potential for small perturbations in one component of the system to lead to disproportionate effects on the overall pain experience, highlighting the limitations of reductionist approaches and the necessity for holistic, multidimensional strategies in pain management and research.
III. Pain is made of thoughts, emotions, and sensation #
One very helpful way of decomposing pain is into a cognitive component (“My back is broken… am I ever going to fix it”?), an emotional component (the unpleasantness of the feeling), and a sensory component (the numb tingling around the lower back).
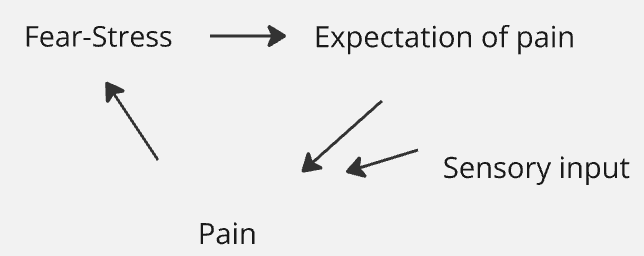
These aspects of pain mutually reinforce each other. Catastrophic thinking can lead to more fear, which heightens the interpretation of the sensation. By recognizing the pain feedback loop and its components, we can often times resolve the pain.
IV. You can change your pain response #
The human brain is capable of incredible adaptation. Blind people can learn to ‘see’ through stimulation on their tongue or echo-location by clicking noises. Stroke survivors who can’t read, speak, or remember can recover and go on to become successful scientists. Severe epileptics can lose the left half of their brain and eventually walk, talk and go to school.
These examples of neuroplasticity demonstrate that our brains can rewire themselves in response to drastic changes. This same plasticity applies to how we process and experience pain. Just as our brains can adapt to loss of sight, they can also learn to recalibrate pain.
There are randomized clinical trials and thousands of anecdotes demonstrating that you can permanently resolve pain through noninvasive procedures7.
There’s no reason a priori that any nervous system cannot recalibrate and resolve the patterns that generate pain. The only question is which stimuli and adjustments will work.
If you want to jump right into working with pain, go to Pain Debugging Protocol. If you have a bit more time for a story, go ahead to Debugging RSI.
-
Downie, Aron, et al. “How common is imaging for low back pain in primary and emergency care? Systematic review and meta-analysis of over 4 million imaging requests across 21 years.” British journal of sports medicine 54.11 (2020): 642-651. ↩︎
-
Jensen, Maureen C., et al. “Magnetic resonance imaging of the lumbar spine in people without back pain.” New England Journal of Medicine 331.2 (1994): 69-73. ↩︎
-
E.g. “‘To anyone looking at me, I have no arm. But I can feel the entirety of my phantom hand and arm. Imagine you are wearing an elbow length evening glove … everywhere the glove touches your skin it’s crushing your arm constantly. … On top of it you get pains like burning pains. It’s like when you burn yourself on the grill. Your instinct is to pull your hand away, but with this pain you can’t. It’s a nerve sensation and it stays there, until “it” decides to pull away’.” Makin, Tamar R. “Phantom limb pain: thinking outside the (mirror) box.” Brain 144.7 (2021): 1929-1932. ↩︎ ↩︎
-
See https://www.who.int/news-room/fact-sheets/detail/low-back-pain They estimate 90% of the reported 619 million of people with lower back pain have nonspecific back pain. 550 million is probably an underestimate. ↩︎
-
See Clauw, Daniel J. “Fibromyalgia: a clinical review.” Jama 311.15 (2014): 1547-1555. ↩︎
-
See Smith, E. S., & Lewin, G. R. (2009). Nociceptors: a phylogenetic view. Journal of Comparative Physiology A, 195(12), 1089-1106. ↩︎
-
RCT examples: Ashar, Yoni K., et al. “Effect of pain reprocessing therapy vs placebo and usual care for patients with chronic back pain: a randomized clinical trial.” JAMA psychiatry 79.1 (2022): 13-23.; Donnino, Michael W., et al. “Psychophysiologic symptom relief therapy for chronic back pain: a pilot randomized controlled trial.” Pain Reports 6.3 (2021): e959. Anecdotes: Patrick Collison: https://x.com/patrickc/status/1559737765566173185, Aaron Iba: https://aaroniba.net/how-i-cured-my-rsi-pain, Josh Comeau: https://x.com/JoshWComeau/status/1379438688602570753, People have cured their pain just by reading Amazon reviews of Sarno’s book: https://x.com/visakanv/status/1652574276531412992 ↩︎